
The Story Behind this year’s Nobel Prize in Physiology and Medicine
Part 1: Going back to Nature
The year is 1967. Thirty-two year old Satoshi Ōmura, in his lab at the prestigious Kitasato University in Japan, is giving serious thought to the direction his research career is going to take. In the two years he has spent at the University, he has studied the structure of multiple antibiotics using nuclear magnetic resonance (NMR) spectroscopy, uncovering information that might go a long way towards elucidating their mode of action. Since the discovery of Penicillin in 1928, the initial rush of antibiotic discovery has died down, and interest has shifted towards figuring out the structure and function of existing antibiotics, so that new drugs can be synthesized chemically based on this data. It is rewarding work for Ōmura, who is a year away from receiving his PhD, but he is not entirely satisfied. More than anything, he is not convinced that the store of medically relevant novel compounds present in the microbial world has been exhausted.
He believes the search is only just beginning.
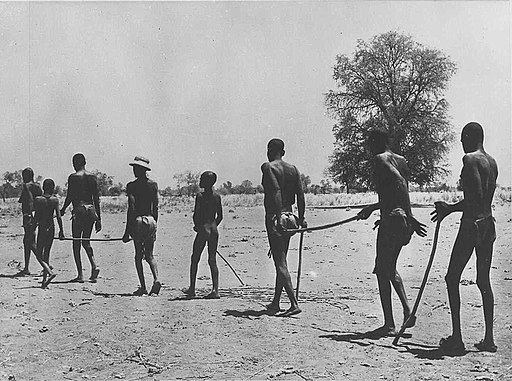
In parts of West and Central Africa, one can find what are sometimes referred to as ‘ghost villages’. These are empty settlements from which the residents have fled, as if fearing some terrible calamity or plague. Surprisingly, these villages are generally found at locations singularly suitable for habitation – close to rivers and next to fertile land.
It is indeed a plague that these villagers have run away from. Those who get infected by it develop severe itches, painful bumps under the skin, and in several cases, permanent blindness. While no one dies from it, those affected often suffer from lifelong affliction and pain, not to mention the loss of their livelihood. And the source of the plague lives right next to the rivers, in these same treacherously fertile lands. You would hardly notice them, the little black flies, as they take their daily blood meals from the unsuspecting villagers who come up to the river to bathe, or simply to carry water back to the village, but their bite carries the tiny organisms that drive entire villages from their homes.
An Unlikely Ally
Four years have passed, and Satoshi Ōmura has settled comfortably into his work in Kitasato University. In this time, he has earned two PhD degrees, one in pharmaceutical sciences, the second in chemistry, and has shifted the focus of his research to the discovery of new antibiotics and novel microbial metabolites from naturally occurring microorganisms. He and his team have devised an array of novel screening assays that have made these discoveries faster, broader, and more efficient. But Ōmura has his eye on the future, and he knows that building international collaborations is the key towards opening up new avenues in antimicrobial research, both for funding and for scope. It is with this goal in mind that when he is granted a sabbatical in September, 1971, he decides to take up a position with Max Tishler, in the Wesleyan University, USA. In 1973, when he returns to Japan, the seeds have been set for a major collaborative effort between the research laboratories of the major pharmaceutical giant Merck and the microbial metabolite team at Kitasato University. The agreement is formalized in April, 1974, with the initial stated focus being the isolation of growth-promoting antibiotics which can be used for livestock farming. In a later amendment, almost as an afterthought, it is decided that the Kitasato University scientists would also ship dried fermented broths which have shown any form of unusual or interesting antimicrobial property to Merck for testing.
The Big Worm and the Small Worm
When a disease-carrying black fly bites a human, it injects microscopic larvae of the parasitic worm Onchocerca volvulus. The larvae migrate to an area just below the skin, and burrow there, slowly growing into adulthood. The adult can live for up to 15 years, and reach nearly half a meter in length. Male and female worms mate in their cozy nodules beneath the skin, and release thousands of tiny larvae, called microfilariae, into the bloodstream each day. The microfilariae quickly spread through the body via the blood, but make sure to travel up close to the skin during daytime, so that feeding blackflies can pick them up and spread them to the next hapless person. The microfilariae are usually around a third of a millimeter in length, and can live for up to two years. When they reach the eye, they can cause an inflammatory response, often leading to permanent blindness. This fact combined with the natural habitat of the black flies has given the disease its common name – River blindness.
Campbell and his Frozen Parasites
Parasitic diseases have plagued humanity since prehistoric times, but in the developed world, the major economic concern they raise is by infecting and affecting the quality of livestock animals. Since the 1930s, Merck had been on the lookout for drugs with antiparasitic activities, and released a few into the market, including Thiabendazole, the first benzimidazole anthelmintic. Other drugs on the market were monensin and hygromycin, released by other pharmaceutical companies. Unfortunately, effectivity was low and new drug discovery was limited by the difficulty of in vivo assays. When William C. Campbell, a parasitologist by training, joined Merck in 1957, he remained on the lookout for assays and compounds that would allow better treatment of parasite infections in humans. Campbell showed that parasitic worms survive freezing in liquid nitrogen, and can be stored in a frozen state for months or even years before revival. This was an important step in the scientific study of parasites, making transportation and time-consuming assays that much easier.
The Elephant Disease
 River blindness is not the only parasitic disease found in sub-Saharan Africa. Microfilariae of the three species – Wuchereria bancrofti, Brugia malayi, and Brugia timori, are carried by mosquitoes, and when transmitted to humans, collect in the lymph nodes following a life cycle very similar to Onchocerca volvulus. While there, they cause inflammation in the lymph nodes, leading to the most grotesque symptom of the disease – edema, which causes body parts to swell up to many times their normal size. It is this feature that gives the disease its most common name – Elephantiasis. According to one estimate, India (the country accounting for 40% of the global cases of lymphatic filariasis) alone suffers a loss of US$ 842 million annually due to lymphatic filariasis.
River blindness is not the only parasitic disease found in sub-Saharan Africa. Microfilariae of the three species – Wuchereria bancrofti, Brugia malayi, and Brugia timori, are carried by mosquitoes, and when transmitted to humans, collect in the lymph nodes following a life cycle very similar to Onchocerca volvulus. While there, they cause inflammation in the lymph nodes, leading to the most grotesque symptom of the disease – edema, which causes body parts to swell up to many times their normal size. It is this feature that gives the disease its most common name – Elephantiasis. According to one estimate, India (the country accounting for 40% of the global cases of lymphatic filariasis) alone suffers a loss of US$ 842 million annually due to lymphatic filariasis.
Near a golf course in Japan…
Among the many microbial cultures that pass through the multiple screening assays in Kitasato under Dr. Ōmura’s supervision, one comes from a soil sample collected near a golf course bordering the ocean in the Shizuoka region of Japan. The isolate is named OS3153, and is forwarded to Merck in 1974 with a batch of 53 other isolates. Merck renames it as MA-4680. In 1975, the broths are sent to the parasitology department for analysis, where they are tested in mice infected with a parasite which models a parasitic infection that affects poultry chicken. The single mouse treated with MA-4680 nearly dies before the scheduled testing. However, it manages to pull through till the confirmatory tests, and the results are astonishing enough to draw attention from Campbell and colleagues. The tests show an extremely potent antiparasitic activity – even a crude extract of unknown concentration is highly effective when added at a concentration of 0.0003% in the feed of the mice. The initial toxicity is shown to be caused by an unrelated agent, and studies are commenced on figuring out the chemistry of this remarkable compound and the biology of the microorganism releasing it, all the while preparing to convert it into a drug for use in livestock. The active component is named Avermectin.

37 million people are infected today with the parasite that causes river blindness. 300,000 of them have been blinded permanently. A further 120 million people are at risk for contracting the disease. 99% of the cases occur in Africa, while a few occur in Yemen and parts of South America. The case with lymphatic filariasis is even worse – over 120 million affected people reside in 73 countries, and a billion people are considered at risk for infection.
The Crucial Years
William C. Campbell submits a proposal to Merck, outlining his desire to use Avermectin for treatment of human diseases caused by parasites. At the forefront of his mind is the African disease river blindness. By this time, a chemical modification of the original Avermectin class of compounds has been shown to lead to a significant increase in efficacy and safety, and the new, modified, semisynthetic drug has been named Ivermectin. Ivermectin has been used on a trial basis in several domestic animals for treatment of parasitic diseases, and has shown promising results. The idea of using it for human trials sticks around for a couple of years, but the data is not considered promising since Avermectin and Ivermectin seem to have little or no effect on adult worms, even though they do get rid of the microfilariae. In 1978, Cambell decides to ask Bruce Copeman, a veterinary parasitologist in Australia to try out Ivermectin in horses to treat a parasitic disorder. This is a significant move, because the horse parasite in question, Onchocerca guttarosa, is closely related to the worms which cause river blindness in humans, and the World Health Organization (WHO) has been showing interest in Copeman’s work from the point of view of treatment of human diseases. By 1979, the data is clear. Ivermectin is capable of completely wiping out the Onchocerca microfilariae. After a series of meetings and conferences with WHO, and considerable wheedling on the part of Campbell, a decision is finally taken to test clinical efficacy of Ivermectin in humans. In 1981-1982, thirty-two infected villagers in Senegal are given a single treatment with Ivermectin. The results speak for themselves. A single treatment with 50 micrograms per Kg of Ivermectin complete eliminates of microfilarial load, with virtually no side effects. The era of Ivermectin has begun.
The next four years saw intensive field trials involving hundreds of thousands of patients from several countries in Sub-Saharan Africa. A single annual dose of Ivermectin was shown to cause complete elimination of microfilaria, an effect lasting up to 12 months after treatment. As the trials drew to a close, it was clear that the results were positive, and the drug was going to be invaluable in fighting these neglected tropical diseases. Merck had a highly successful, potentially life-giving drug on its hands. The only things that remained to be decided were the price and the marketing.
In 1987, Merck announced that they were going to provide the drug Ivermectin completely free of charge, for ‘as long as it is needed’ for the treatment of river blindness. This was met with full consent from the group at Kitasato University who agreed to forgo all royalties. It was an unprecedented and extraordinary move, which remains till date one of the biggest drug donation campaigns ever started. Over the last 25 years, over 200 million people, many of them extremely poor villagers from Sub-Saharan Africa have received Ivermectin treatment. In 1998, the donation effort was expanded to include the parasitic disease lymphatic filariasis, and over 118 million people have received treatment since then. This donation effort transformed the treatment of river blindness and lymphatic filariasis, to the point that WHO is now envisioning complete eradication of the diseases by 2025 and 2020 respectively. In several of the ‘ghost villages’ in Africa, people have started returning to their homes.
The discoverers have continued work in the meanwhile, trying to figure out the mode of action and the mechanism of synthesis of this remarkable drug. In spite of repeated isolation efforts, Streptomyces avermitilis, the original bacteria from the soil sample collected in Japan remains the only known species to synthesize Avermectin. Avermectin and Ivermectin were the first compounds known to act on both ecto and endoparasites, putting them in the class ‘endectocide’, a class that had to be invented to accommodate these drugs. While the exact mode of action of Avermectin/Ivermectin is not known in detail, it is believed that they might act by inhibiting neurotransmitter gated chloride channels in the worm, paralyzing its muscles and shutting down its nervous system, resulting in a slow death which does not cause an inflammatory response.
Satoshi Ōmura continued indulging his love for microbial metabolites, and has spent more than 45 years in the field, isolating, characterizing and utilizing various bioactive compounds produced by these tiniest of organisms. William Cambell continued work with Merck till 1990, spending 33 years with the company, before taking up a position as Research Fellow Emeritus at Drew University, Madison, USA . Today, Ōmura is 80, Campbell is 85, and both remain active in the fields which claimed their passion so many years ago. Ōmura is an accomplished cross-country golfer, while Campbell continues to play ping-pong thrice a week.
On 7 Nov, 2015, the Nobel Committee announced that one half of the 2015 Nobel Prize in Physiology is going to be awarded to Satoshi Ōmura and William C. Cambell for “for their discoveries concerning a novel therapy against infections caused by roundworm parasites“. In his acknowledgment of the award, Campbell stressed on how much of a team effort the discovery of Avermectin was, and how this award recognized a unique public sector-private sector collaboration which has achieved so much for human health in so short a time.
Part 2: Looking Back at History



On 4th October, 1971, about a month after Satoshi Ōmura left from Japan for the USA, the results were back. The new extract showed 100% efficacy against the parasite, and completely abolished parasitemia in both mice and monkeys infected with Plasmodium.

Here, once more, world history intervenes on what should have been a purely scientific story. The findings of the Project 523 team were published internally and in several Chinese journals, but due to the prevailing political climate, little of it leaked into the outside world. The project was carried out in secrecy and the researchers involved were not allowed to publish their findings outside China. The turning point came in 1981, when project 523 was officially terminated. The same year, the World Health Organization held a conference in Beijing, China, and Tu Youyou was allowed to present her findings before the world.
It took several years, and a stubborn insistence upon multiple other field trials, before Artemisinin was adopted for widespread use outside China. In 2005, WHO recommended Artemisinin combination therapies (ACT) for treatment of malaria in huge portions of sub-Saharan Africa. According to a WHO report, between 2000 and 2013, mortality rate due to malaria has dropped by 47%, and the number of infections have dropped by 26%. Artemisinin based therapies, when combined with insecticidal strategies, is believed to have contributed strongly to this downward trend.
The second half of the 2015 Nobel Prize in Physiology and Medicine was awarded to Tu Youyou for “for her discoveries concerning a novel therapy against Malaria“. She is only the twelfth woman and the first Chinese citizen to be awarded the Nobel Prize in Physiology and Medicine in its 115 year old history (She is the 49th woman and 8th Chinese to win a Nobel overall). Tu Youyou, now 85 years old, remains an active member of the China academy of Chinese Medical Sciences.
Together, the drugs Artemisinin and Avermectin (and its derivative Ivermectin) are estimated to have impacted over a billion people worldwide, most of them in extremely poverty-stricken areas. Through their inspired research, these three extraordinary individuals made a lasting contribution towards global health, and truly deserve all the honors and accolades coming their way.
————————————————————————————————————————
References and further reading –
- Nobel Committee’s press release and scientific background
- Four wonderful reviews –
- Tu Y. The discovery of artemisinin (qinghaosu) and gifts from Chinese medicine. Nat Med 2011;17:1217–1220.
- Ōmura S. Microbial metabolites: 45 years of wandering, wondering and discovering. Tetrahedron 2011;67:6420–6459.
- Õmura S, Crump A. Timeline: The life and times of ivermectin — a success story. Nat Rev Microbiol 2004;2:984–989.
- Campbell WC. History of Avermectin and Ivermectin, with Notes on the History of Other Macrocyclic Lactone Antiparasitic Agents. Curr Pharm Biotechnol 2012;13:853–865.
